Aaron Trinidade, FRCS (ORL-HNS)
ENT Surgeon
Providing exceptional care for your ears, nose & throat

Helen Frankel: 07968312069
Private Secretary
Tonsillitis & glandular fever
What is tonsillitis?
Tonsillitis is in infection of the tonsils. Because of their relatively exposed position, tonsils are prone to developing infections. Tonsillitis is the most common of these and is usually viral, but may be bacterial.
What are the symptoms?
A sore throat is the main symptom, followed by difficulty swallowing and a general feeling of being run down (called malaise). You may develop a fever as well.
How is it diagnosed?
Your GP can usually diagnose it based on the symptoms and examination of the back of the throat. Usually, the doctor can tell whether tonsillitis is viral or bacterial based on what the tonsils look like. Generally, in viral tonsillitis the tonsils are simply red, swollen and inflamed and the patient may have a low-grade fever, whereas bacterial tonsillitis is often accompanied by white patches (called exudates) on the surface of the tonsils and higher fevers. There are no specific tests for tonsillitis. Sometimes a throat swab is performed to find out what bug is causing the infection, but this does not usually change how the tonsillitis is treated and is often not necessary.
What is glandular fever?
Glandular fever is a disease caused by the Epstein-Barr virus (EBV) and is also called infectious mononucleosis. It affects the whole body, causing extreme malaise, fever, swelling of the neck glands (lymph nodes) and tonsillitis. It is the tonsillitis that usually brings people to the doctor. The tonsils are typically coated with a thick, white, continuous layer of slough (pronounced: sluff). Symptoms generally last 1 to 2 weeks and are treated with supportive measures.
Because glandular fever affects the entire body, in some cases the liver and spleen can also swell and become exposed from their protective position behind the rib cage. Your doctor or ENT surgeon can examine the abdomen to see if this has occurred. In these cases, it is usually advised that activities such as contact sports are avoided for 4 to 6 weeks to allow time for the swelling to subside as a blow to the abdomen may cause injury to these organs.
How is glandular fever diagnosed?
Glandular fever is usually diagnosed based on the symptoms, examination of the tonsils and a blood test called a Monospot test.
How are tonsillitis and glandular fever treated?
Viral tonsillitis often settles spontaneously within a week without the need for antibiotics (which do not work on viruses) and most cases can be treated with supportive measures such as good hydration and pain relief.
Bacterial tonsillitis usually requires an antibiotic in addition to supportive measures. Sometimes admission to the hospital is necessary in cases where further pain relief is required or in cases where the patient cannot swallow and requires intravenous fluid hydration.
In glandular fever, admission to the hospital is also sometimes required in cases where further pain relief is required or in cases where the patient cannot swallow and requires intravenous fluid hydration. Although glandular fever is viral, antibiotics may be added to prevent a secondary bacterial infection of the tonsils.
In all cases of tonsillitis, infection may lead to swelling at the back of the throat, which can rarely lead to a difficulty in breathing. In such cases, a short course of steroids may be administered to help reduse this swelling.
When is tonsillectomy indicated for tonsillitis?
Tonsillectomy (removal of the tonsils) can be performed for recurrent tonsillitis (including glandular fever). Most doctors and ENT surgeons refer to the Scottish Intercollegiate Guidelines Network (SIGN) guidelines on tonsillitis to decide when the tonsils should be removed. The guidelines state that tonsillectomy can be considered when:
-
Sore throats are due to tonsillitis (and not other causes such as pharyngitis)
-
The episodes of sore throat are disabling and preventing normal functioning
-
There have been 7 episodes of well-documented, disabling tonsillitis in the preceding year, OR
-
There have been 5 episodes of well-documented, disabling tonsillitis in the preceding 2 years, OR
-
There have been 3 episodes of well-documented, disabling tonsillitis in the preceding 3 years
These are guidelines only and exceptions sometimes made on a case by case basis. However, most cases of recurrent tonsillitis (75%) will resolve by 1 year with no need for surgery. If there is doubt about whether someone has developed recurrent tonsillitis, a 6-month period of watchful waiting can be undertaken, during which time the patient or parent can keep a diary of all episodes during that time. This can be helpful in making a decision about whether to progress to a tonsillectomy or not. Mr Trinidade can further discuss whether tonsillectomy is right for you or your child.
More information
The SIGN guidelines can be read in full here.
For more information on tonsillectomy, click here.
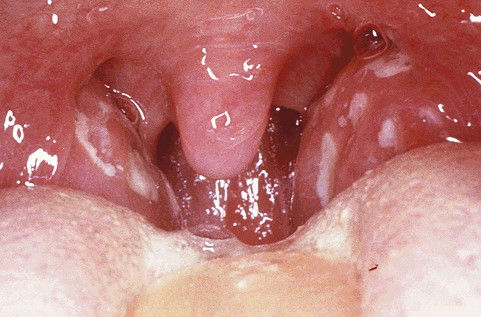
Bacterial tonsillitis showing exudates on the surface of the tonsils

The tonsillitis associated with glandular fever showing thick, white, continuous slough on the surface of the tonsils

