Aaron Trinidade, FRCS (ORL-HNS)
ENT Surgeon
Providing exceptional care for your ears, nose & throat

Helen Frankel: 07968312069
Private Secretary
Adenoids & adenoidectomy
What are adenoids?
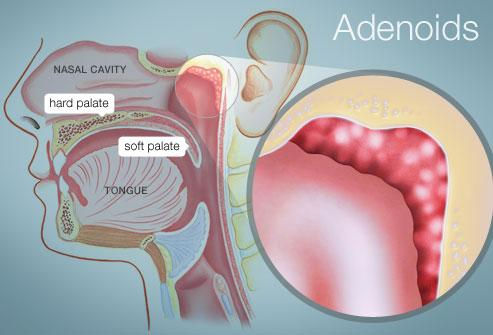
The adenoids are an area of soft tissue at the back of the nose. They are made of lymphoid tissue, the same tissue as tonsils are, and, like tonsils, are part of the immune system. They can be thought of as tonsils at the back of the nose.
Do they have a function?
Because of their position at the back of the nose, adenoids are one of the first areas to be exposed to viruses and bacteria that might be inhaled in during breathing. Once exposed, they send signals to the rest of the immune system to initiate a response to potential infection, and therefore act as a first line of defence against infection. In this way, the immune system matures and can prepare itself for similar infections more quickly and efficiently in the future (tonsils at the back of the throat function in a similar way). As very young children such as toddlers are being exposed to various viruses and bacteria for the first time (especially when they start daycare where they are exposed to more bugs from other children), their adenoids tend to be much larger than in other age groups, but as the child’s immune system matures, adenoids tend to get smaller as the child gets older, typically disappearing altogether by the age of 9 to 12 (although they may sometimes persist into adulthood). Adenoids are not thought to have much function in children past the age of 2 or 3 and removing them makes no difference to a child’s long term immunity or ability to fight infection.
The adenoids, together with the soft palate (the back part of the roof of the mouth), also serve to help block off the back of the nose from the mouth during swallowing and so prevent regurgitation of food and fluids into the nose. This role of the adenoids is more important in younger children and in children with cleft palate where the palate is weakened. The importance of the adenoids in preventing nasal regurgitation reduces as the child gets older and the soft palate either strengthens, or, in the case of cleft palate, is surgically repaired.
What kind of problems can adenoids cause?
Adenoids usually cause problems when they are enlarged and therefore mainly give problems in young children, as they are the age group most likely to have enlarged adenoids for reasons explained above. The main problems include nasal obstruction causing mouth breathing, a constantly runny nose, a nasal voice, snoring and even sleep apnoea at night. These problems tend to get worse when the child has a cold.
Because the adenoids sit in between the openings of the Eustachian tubes (the tubes that help to ventilate the middle ear), when they are enlarged, they can block these tubes. Viruses and bacteria within the inflamed adenoids can also travel up the the Eustachian tubes and cause inflammation in the middle ears. The combined result of this blockage and inflammation is a build up of fluid in the middle ear, known as otitis media with effusion (glue ear). This can cause hearing difficulty and other symptoms. The fluid may also get infected, resulting in acute otitis media (middle ear infection).
How is a problem with the adenoids diagnosed?
Most cases of problematic adenoids are reliably diagnosed based on the symptoms that the child is suffering with. Sometimes the adenoids can be viewed with an endoscope (a type of telescope) inserted into the nose, but this is usually only tolerated by some older children. Occasionally they can be seen by simply shining a torch up the nostrils, but does not give an accurate representation of the size of the adenoids. If there is doubt about the diagnosis, an X-ray of the head can sometimes show enlarged adenoids, but is not always reliable, especially in very young children.
How are problematic adenoids treated?
This will depend on the age of the child and the severity of the symptoms. For children who have only mild problems or only get symptoms when they have a cold, then a conservative non-surgical approach can be taken. This usually involves the use of a medicated nasal spray (such as Flixonase or Nasonex), saline drops into the nose or both, especially in children who are known to have allergies or hayfever. These sprays can be used regularly or as needed until the child’s adenoids naturally shrink as he or she gets older. Antibiotics are not generally useful in adenoidal problems, but are sometimes considered.
When should a child with problematic adenoids have them removed?
Removal of the adenoids (adenoidectomy) is considered in the following circumstances:
-
When they are causing a disruption of sleep due to snoring and sleep apnoea (usually the tonsils are removed at the same time)
-
As part of the treatment of glue ear or recurrent middle ear infections (especially if the child has nasal symptoms; grommets are usually inserted at the same time)
-
Persistent nasal blockage and runny nose affecting the child’s quality of life
-
Some surgeons remove adenoids at the same time as tonsils as part of the treatment for recurrent tonsillitis
Mr Trinidade can discuss with you whether adenoidectomy is right for your child.
How is an adenoidectomy performed?
Adenoidectomy is performed under general anaesthetic, usually as a day case procedure, with the child being allowed home the same day, but overnight admission in hospital may sometimes be required in children who have severe symptoms, other medical problems, or live more than 30 minutes from the hospital. The procedure lasts 15 to 20 minutes.
The adenoids are removed through the mouth in a similar way to tonsils during tonsillectomy. They are removed either using the curettage method, in which a metal instrument (a curette) is passed through the mouth, around the back of the soft palate and into the back of the nose where they are used to scrape the adenoids away. Electrocautery can also be used, in which an electric probe (suction diathermy) is used through the mouth, instead of a curette, to cauterize (burn) and shrink the adenoids away. In cases of very large adenoids, both methods are sometimes used. Bleeding is then stopped using temporary packs at the back of the nose (removed before the child wakes up) and cautery. Both curettage and electrocautery methods are equally effective. Mr Trinidade has been trained to use both methods.
What are the risks of adenoidectomy?
Adenoidectomy is a commonly performed procedure in children and the majority are performed risk-free. However, there are some risks to be aware of. The main risk of adenoidectomy is a small risk of bleeding post-operatively (1 to 2%). If this occurs, it is often light bleeding but can sometimes be heavy and require further surgery to stop the bleeding. A clotting disorder or a family history of one can increase the risk of bleeding.
Teeth can sometimes be chipped or knocked loose during instrumentation of the mouth. Usually these teeth are already loose (milk teeth or teeth with cavities). Rarely they can be inhaled into the lungs after being knocked loose and an additional procedure (a bronchoscopy, which is a telescope inserted down the windpipe) needs to be performed to retrieve the lost tooth.
Sometimes, the symptoms that adenoidectomy was performed for can persist after the operation. This may mean that there were other factors at play and that the adenoids were only part of the problem (for example, enlarged adenoids AND rhinitis in a child with nasal blockage). Other treatments may need to be used in addition to the adenoidectomy in such cases to achieve success. In other cases, symptoms can return even after an initially successful adenoidectomy. This may indicate regrowth of the adenoids, and usually occurs several months after the original operation (adenoids can grow back, unlike tonsils, which do not). In these cases, revision adenoidectomy may be required.
In rare cases, a child is more dependent than usual on the adenoids for blocking the nose off during swallowing and preventing regurgitation of food and drink into the nose. In this case, removal of the adenoids can leave the child prone to nasal regurgitation as the soft palate cannot efficiently close off the nose on its own. A hissing noise may also be heard when the child speaks due to air escaping through the nose during speech. This is known as velopalatine insufficiency, and often resolves on its own with time as the soft palate strengthens, but can require surgical correction in some cases. Velopalatine insufficiency is more common in children with a history of cleft palate or other palate problems.
Should a child with a history of cleft palate have an adenoidectomy?
Children with cleft palate have an inherently weakened soft palate, even after repair, and are therefore more dependent on the adenoids to help maintain nasal closure during swallowing. For this reason, adenoidectomy in these children is best avoided where possible. If the adenoids are problematic and are not responding to non-surgical treatments, then in selected cases they can still be considered for removal, with a partial adenoidectomy being performed instead, where only the obstructing part of the adenoids is removed and a portion is left behind that continues to help the soft palate in its function. This can help to reduce the risk of velopalatine insufficiency in these children and the electrocautery method of adenoidectomy is usually used as it is more precise in these situations. Children with cleft palate who have persistently problematic adenoids are best assessed by an ENT surgeon with a sub-specialist interest in paediatric ENT.
What is the post-operative care following adenoidectomy?
Your child may experience some discomfort at the back of the nose for a few days, which is usually controlled with paracetamol and ibuprofen. There may be a period of halitosis (bad breath) for a few days due to some dead tissue at the back of the nose, which eventually disappears. This usually occurs if the electrocautery method is used. Antibiotics are sometimes prescribed if infection is suspected. Children should be encouraged to resume a normal diet and normal activities as soon as possible after the operation (usually 1 to 2 days).
Some bleeding mixed with mucus is not uncommon after adenoidectomy and quickly settles after the first day following surgery. Parents should observe for any signs of heavier bleeding, however, which may present either as a nose bleed or bleeding from the mouth. Sometimes, bleeding occurs as a slow drip down the back of the throat that the child swallows over time and then vomits up all at once. The vomit has the appearance of coffee grounds and represents digested blood. In all of these cases, the child should be immediately taken to the nearest A&E Department for stabilization, assessment and management by the ENT surgeon on call. Call an ambulance if necessary. The child should not be given anything to eat or drink as he or she may need to be taken to the operating room urgently to have the bleeding stopped. Most cases of problematic bleeding will settle on their own with only observation and intravenous antibiotics and fluids, however.
Most cases of adenoidectomy recover with no issue and children can return to nursery or school after 5 to 7 days.